
Trabeculectomy
Trabeculectomy is an operation to lower the pressure in the eye. It is performed by creating a small channel in the wall of the eye which is covered by a thin trap door flap.
Download printable information sheet
Languages: English, Arabic, Greek, Portuguese, Spanish
FAQ
Frequently Asked Questions
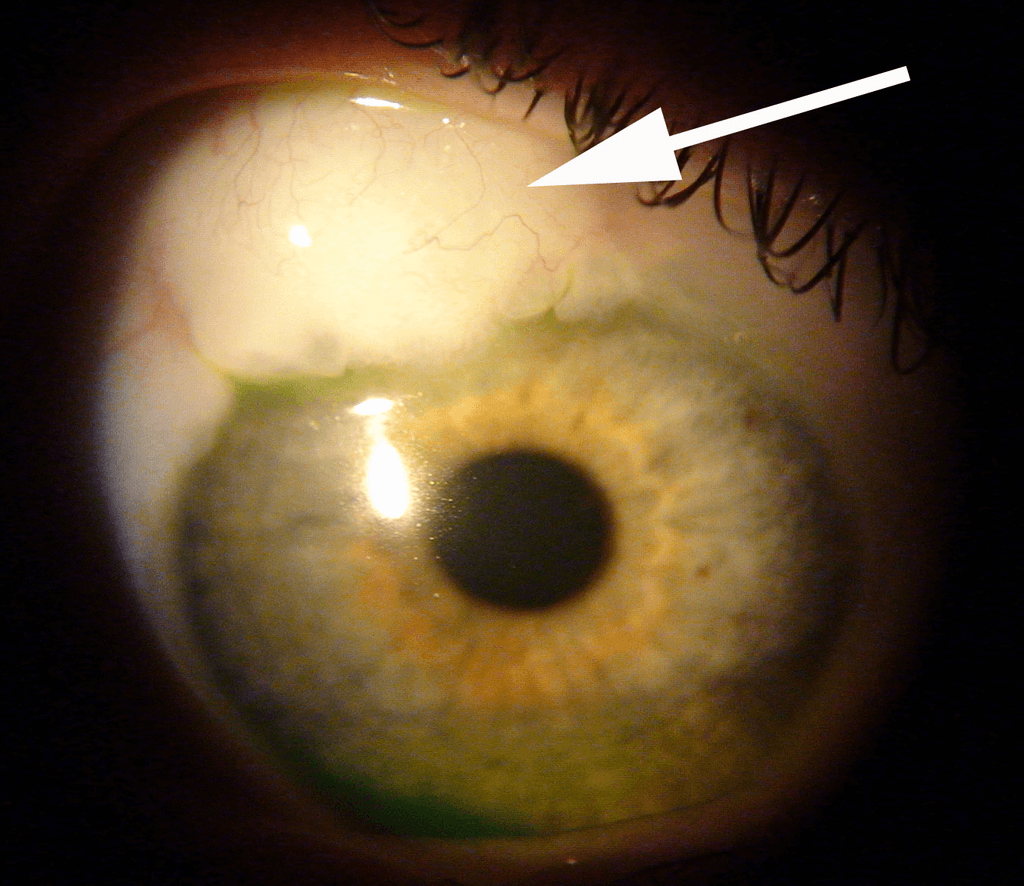
Trabeculectomy is a surgical operation which lowers the pressure inside the eye (intraocular pressure) in patients with glaucoma. This is achieved by making a small hole in the eye wall (sclera), covered by a thin trap‐door in the sclera. The fluid inside the eye known as aqueous humor, drains through the trap‐door to a small reservoir or bleb just under the eye surface, hidden by the eyelid (see below). The trap‐door is sutured (stitched) in a way that prevents aqueous humor from draining too quickly.
By draining aqueous humor the trabeculectomy operation reduces the pressure on the optic nerve and prevents further damage and further loss of vision in glaucoma.
Please note that control of the eye pressure with a trabeculectomy will not restore vision already lost from glaucoma.
The aqueous humor is a fluid inside the eye and is not related to the tears. Watering of the eye is caused by tears, not aqueous humor. Glaucoma is often caused by high pressure in the aqueous humor inside the eye. Trabeculectomy reduces the eye pressure by draining aqueous humor from the eye.
The aqueous humor that drains through the trabeculectomy accumulates in a reservoir between the sclera and the surface layer of tissue that covers the eyeball (the conjunctiva) to form a small drainage bleb that is usually hidden under the upper eyelid.
Initially the eye will be red and swollen to a variable degree after surgery. The eyelid may also droop partially. This resolves over a period of weeks to months. The drainage bleb is not usually visible to the naked eye after the trabeculectomy operation. The bleb may, however, be seen if the patient looks in the mirror and raises the upper eyelid. After surgery, most patients feel no sensation from the presence of the drainage bleb. Rarely, patients are aware of the drainage bleb. Should this occur, steps can be taken to make the bleb more comfortable; this is discussed further under complications.
Prior to undergoing surgery, patients are asked to continue all drops and tablets in accordance with their normal treatment regimen until the morning of the operation. Blood thinning medications such as Aspirin, Warfarin and Clopidogrel should also be continued. Patients who are taking Warfarin are advised to have their level (eg. INR) checked at least 2 weeks prior to surgery to ensure it is within the correct therapeutic range.
If patients opt to have the surgery performed under general anaesthesia, a preoperative assessment of their general health will be carried out just before surgery. Underlying medical conditions including cardiac disease, uncontrolled high blood pressure or diabetes will need to be addressed prior to scheduling of surgery.
Anaesthesia
Trabeculectomy is often performed under local anaesthesia, though it may also be performed under general anaesthesia.
Patients who have their surgery under local anaesthesia will be awake during the operation but will have the option of requesting light sedation. The eye will be anaesthetised first with eye drops and then an injection of anaesthetic will be administered around the eye. The anaesthetic injection itself may cause some mild discomfort; a slight sensation of pressure as the anaesthetic is delivered. The injection anaesthetises the eye, preventing not only pain but also excessive eye movement during surgery. During surgery patients are covered by a sterile sheet, or drape, which keeps the operation site sterile and also prevents patients from seeing any of the surgery. Patients will be aware of the surgeon working around the eye, but should not feel pain. In the event of any pain or discomfort, the patient may calmly raise a hand and the surgeon will stop the surgery and top‐up the anaesthetic if needed. Patients may also hear the surgeon speaking to the scrub nurse and other members of the surgical team.
Mitomycin C
During the surgery, Mitomycin C may be applied to the surface of the eye for a brief period of time (usually 2‐3 minutes). Mitomycin C is a drug that was originally used to treat cancer, but it is also used in glaucoma surgery to reduce scarring. Scarring prevents the trabeculectomy from functioning in the long term, as it prevents the aqueous humor from being absorbed back into the circulation. The Mitomycin C is then washed away from the eye with sterile water so that no residual drug remains.
Patients are usually discharged home from hospital either the same day as the surgery or the day after.
The eye is normally padded after surgery and the eye pad is removed the following day. If the unoperated eye does not see well, then the operated eye will not be padded. Instead, a clear shield will be placed on the operated eye so that it is still possible to see after surgery.
It is normal for the vision to be blurred and the eye to be uncomfortable after surgery. The period of blurring is variable. The vision may be particularly blurred for 1‐2 weeks following surgery, and then start to improve. It can take 2‐3 months for the eye to feel completely normal and the vision to stabilise completely.
You may be asked to wear an eye shield at night for the first 2 weeks or so; this is to prevent any accidental harm to the operative site whilst sleeping.
Soreness in the eye after surgery is partly due to the surgery itself, and partly due to the stitches (or sutures). The sutures do not dissolve and are usually removed in the clinic 2 to 3 weeks after surgery (this takes 2 – 3 minutes in clinic with the eye anaesthetised using eye drops). The eye usually starts to feel more comfortable after the sutures have been removed.
Patients are usually seen once weekly for the first 4 weeks, and may be seen more frequently if the eye pressure is either too high or too low.
During this time sutures may be removed to adjust the pressure and additional injections of steroids or 5‐Fluororacil (a drug that reduces healing), may be given around the eye to counteract the body’s natural healing process. The injections are performed after the administration of anaesthetic eyedrops, during the clinic appointment itself.
Eye drops will be prescribed to use regularly after surgery. These start the day after surgery, after the post‐operative examination. It is not usually necessary to use eye drops the first night after the surgery. Acetazolamide (Diamox) tablets or any glaucoma medication to the operated eye should also be stopped the night after surgery unless advised otherwise.
It is important that any eye drops for the unoperated eye are continued unless advised otherwise.
The postoperative eye drops will usually consist of an antibiotic and anti‐inflammatory steroid. The steroid eye drop will initially be used intensively (every 2 hours or about 8 times daily) and the antibiotic four times daily. The postoperative eye drops will normally need to be taken for 2 to 3 months and the dose will be adjusted by your doctor.
It is important to avoid strenuous activity during the early post‐operative period including swimming, tennis, jogging and contact sports.
It is permissible to watch television and read, as these will not harm the eye. Bending over however can cause significant pain when the eye is still inflamed after surgery. Similarly, activities such as yoga that require head‐down posturing should be avoided.
If the eye pressure is very low after surgery, your surgeon may suggest refraining from all exertion and remaining sedentary until the pressure is restored.
In most cases, it takes 2 to 3 months for the eye to feel completely normal and sometimes longer in more complicated cases. At this point a refraction (spectacle test) is usually required as the spectacle prescription may have changed slightly from the pre‐surgery prescription.
Severe complications are rare and may happen either if the eye pressure drops very low or very quickly during the early postoperative period, or if the eye becomes infected.
Very low eye pressure is the biggest risk in the early postoperative period. Although it is often painless, it may be associated with a dull aching feeling or a throbbing sensation within the operated eye. Patients who notice severe blurring of vision, distortion or a fluctuating curtain in their visual field should attend the eye casualty department as soon as possible for further assessment.
Very low pressure or a precipitous drop in pressure can result in bleeding at the back of the eye (choroidal haemorrhage). This is a very severe complication but rare. In order to ensure that this does not happen the surgeon will often suggest further intervention if the pressure becomes very low. Such intervention may consist of a return to the operating theatre to have the trap‐door sutures tightened. Sometimes the surgeon will inject a viscoelastic gel into the eye and wait to observe the result before deciding on further adjustment of the trap‐door sutures, as the eye pressure will often stabilise by itself. Sometimes a simple adjustment of medication is sufficient, in which case, neither of the above will be required.
The longer‐term risks of trabeculectomy are infection, discomfort, cataract and change in glasses prescription. Low pressure occasionally develops in the longer term, but generally the risk of low pressure is highest in the early postoperative period rather than later.
Editors
Founding Editors
MIGS.org was developed by glaucoma surgeons with a broad experience in minimally invasive glaucoma surgery to provide patients with evidence-based and unbiased information.


Glaucoma Specialist
Dr Nathan Kerr



